Impact of the COVID-19 Pandemic on Urological Care Delivery in the United States
Research Lead:
Daniel J Lee, Jeremy B Shelton, Paul Brendel, Rahul Doraiswami, Danil Makarov, William Meeks, Raymond Fang, Matthew T Roe, Matthew R Cooperberg
- PMID: 34470508
- PMCID: PMC8584199
- DOI: 10.1097/JU.0000000000002145
Abstract
Purpose: We examined changes in urological care delivery due to COVID-19 in the U.S. based on patient, practice, and local/regional demographic and pandemic response features.
Materials and methods: We analyzed real-world data from the American Urological Association Quality (AQUA) Registry collected from electronic health record systems. Data represented 157 outpatient urological practices and 3,165 providers across 48 U.S. states and territories, including 3,297,721 unique patients, 12,488,831 total outpatient visits and 2,194,456 procedures. The primary outcome measure was the number of outpatient visits and procedures performed (inpatient or outpatient) per practice per week, measured from January 2019 to February 2021.
Results: We found large (>50%) declines in outpatient visits from March 2020 to April 2020 across patient demographic groups and states, regardless of timing of state stay-at-home orders. Nonurgent outpatient visits decreased more across various nonurgent procedures (49%-59%) than for procedures performed for potentially urgent diagnoses (38%-52%); surgical procedures for nonurgent conditions also decreased more (43%-79%) than those for potentially urgent conditions (43%-53%). African American patients had similar decreases in outpatient visits compared with Asians and Caucasians, but also slower recoveries back to baseline. Medicare-insured patients had the steepest declines (55%), while those on Medicaid and government insurance had the lowest percentage of recovery to baseline (73% and 69%, respectively).
Conclusions: This study provides real-world evidence on the decline in urological care across demographic groups and practice settings, and demonstrates a differential impact on the utilization of urological health services by demographics and procedure type.
Keywords: COVID-19; health services research; healthcare disparities; socioeconomic factors; urology.
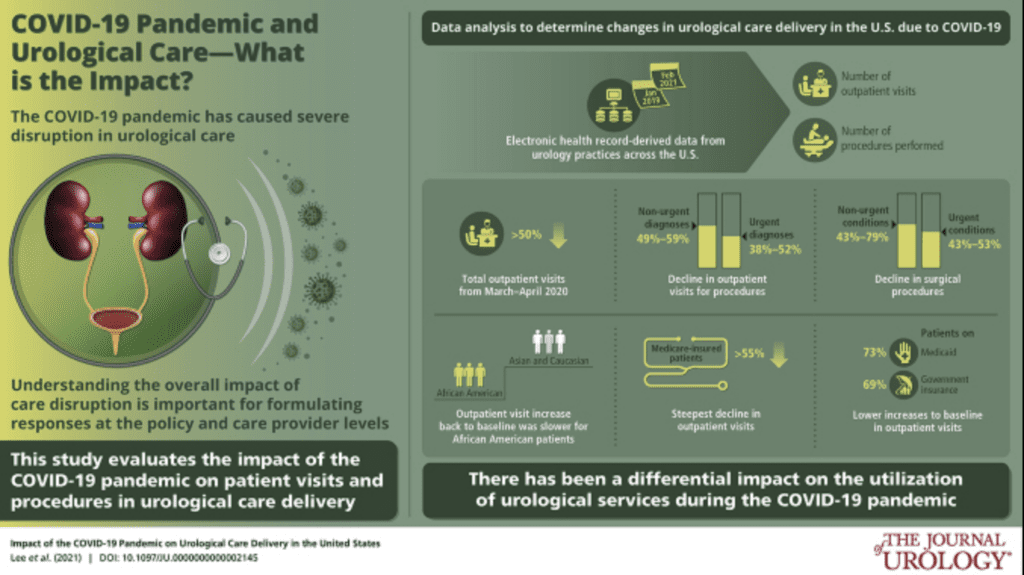
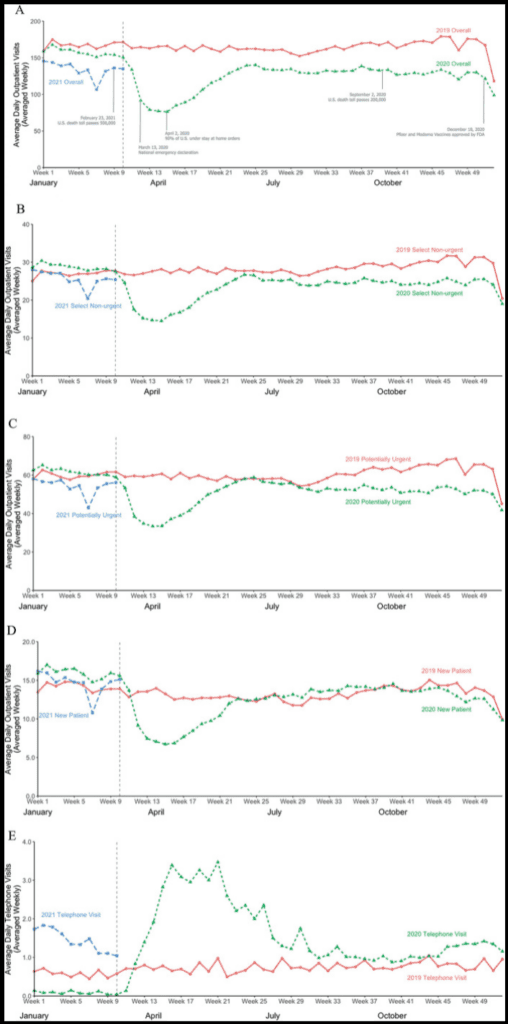
Figure.
A to E, weekly average of outpatient clinic visits from January 2019 to February 2021 per practice for overall population (A), select nonurgent diagnoses (B), potentially urgent diagnoses (C), new patient visits (D), and telephone visits (E). Nonurgent subset included microscopic hematuria, overactive bladder, elevated prostate specific antigen, erectile dysfunction and BPH (B). Urgent subset included prostate cancer, bladder cancer, kidney cancer, kidney stones, urinary tract infection, gross hematuria and renal mass (C). Beginning in March 2020 (week 10), there was sharp, nearly 50%, decrease in total outpatient visits, which reached nadir in April (week 15), with rebound period stretching from May to June (weeks 16 to 24) and reaching 92% of baseline, followed by another decrease, with visits at 77% of baseline.
References
- Cutler D: How will COVID-19 affect the health care economy? JAMA 2020; 323: 2237. – PubMed
- McWilliams JM Mehrotra A and Russo A: Implications of early health care spending reductions for expected spending as the COVID-19 pandemic evolves. JAMA Intern Med 2021; 181: 118. – PMC – PubMed
- Fu SJ, George EL, Maggio PM, et al. : The consequences of delaying elective surgery: surgical perspective. Ann Surg 2020; 272: e79. – PMC – PubMed
- Shelton JB, Pichardo D, Meeks W, et al. : Characteristics of participants in the American Urological Association Quality (AQUA) Registry and early impact of participation on quality of care. Urol Pract 2021; 8: 209.
- USDA ERS: Rural-Urban Commuting Area Codes. U.S. Department of Agriculture 2019. Available at https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Accessed June 28, 2021.
- Trump DJ: Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19). The White House; 2020. Accessed December 19, 2020.
- Health Resources and Service Administration. Department of Health and Human Services: HRSA Data Warehouse. Department of Health and Human Services; 2020. Available at https://data.hrsa.gov/data/download. Accessed December 12, 2020.
- American Urological Association: Covid-19 Info Center. American Urological Association; 2020. Accessed December 21, 2020.
- Jung RG, Di Santo P, Clifford C, et al. : Methodological quality of COVID-19 clinical research. Nat Commun 2021; 12: 943. – PMC – PubMed
- Austin JM and Kachalia A: The state of health care quality measurement in the era of COVID-19: the importance of doing better. JAMA 2020; 324: 333. – PubMed
- Alexander GC, Tajanlangit M, Heyward J, et al. : Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open 2020; 3: e2021476. – PMC – PubMed
- Wright AL, Sonin K, Driscoll J, et al. : Poverty and economic dislocation reduce compliance with COVID-19 shelter-in-place protocols. J Econ Behav Organ 2020; 180: 544. – PMC – PubMed
- Clapp J, Calvo-Friedman A, Cameron S, et al. : The COVID-19 shadow pandemic: meeting social needs for a city in lockdown. Health Aff (Millwood) 2020; 39: 1592. – PubMed
- Ogedegbe G, Ravenell J, Adhikari S, et al. : Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York city. JAMA Netw Open 2020; 12: e2026881. – PMC – PubMed
- Muñoz-Price LS, Nattinger AB, Rivera F, et al. : Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open 2020; 3: e2021892. – PMC – PubMed
- Rubin R: COVID-19’s crushing effects on medical practices, some of which might not survive. JAMA 2020; 324: 321. – PubMed
- Coleman-Lochner L: Hospitals risk bankrupty in latest COVID wave. Bloomberg 2020. https://www.bloomberg.com/news/articles/2020-10-14/shaky-u-s-hospitals-r…. Accessed December 19, 2020.
- Gaither TW, Awad MA, Fang R, et al. : The near-future impact of retirement on the urologic workforce: results from the American Urological Association Census. Urology 2016; 94: 85. – PubMed
- Eberly LA, Kallan MJ, Julien HM, et al. : Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open 2020; 123: e2031640. – PMC – PubMed
- Kwok CS, Gale CP, Kinnaird T, et al. : Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 2020; 106: 1805. – PubMed
- Gawron AJ Kaltenbach T and Dominitz JA: The impact of the coronavirus disease-19 pandemic on access to endoscopy procedures in the VA healthcare system. Gastroenterology 2020; 159: 1216. – PMC – PubMed
- Whaley CM, Pera MF, Cantor J, et al. : Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open 2020; 3: e2024984. – PMC – PubMed
- Patt D, Gordan L, Diaz M, et al. : Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform 2020; 4: 1059. – PMC – PubMed
- Maringe C, Spicer J, Morris M, et al. : The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020; 21: 1023. – PMC – PubMed
- Woolf SH, Chapman DA, Sabo RT, et al. : Excess deaths from COVID-19 and other causes, March–July 2020. JAMA 2020; 324: 1562. – PMC – PubMed
- Cisternas AF, Ramachandran R, Yaksh TL, et al. : Unintended consequences of COVID-19 safety measures on patients with chronic knee pain forced to defer joint replacement surgery. Pain Rep 2020; 5: e855. – PMC – PubMed
- Bekelman JE Emanuel EJ and Navathe AS: Outpatient treatment at home for Medicare beneficiaries during and after the COVID-19 pandemic. JAMA 2020; 324: 21. – PubMed
- Laughlin A, Begley M, Delaney T, et al. : Accelerating the delivery of cancer care at home during the Covid-19 pandemic. NEJM Catalyst 2020. doi: 10.1056/CAT.20.0258. – DOI

Talk to a Qdata Expert
Take a minute to submit your contact information and one of our team members will reach out to you.